Pasture: Is it Affecting Behaviour?
Is Pasture Affecting Your Horse’s Behaviour?
During times of the year when pasture is young, lush, very green and growing quickly it is common to find horse owners having problems with their horse and particularly their behaviour. Normally quiet, calm horses can become ‘spooky’, behave erratically and become excited easily, show signs of incoordination, muscle tenseness, soreness or twitching and in severe cases may become dangerously aggressive and exhibit unusual herding behaviour. Some people refer to their horses as “grass affected” when this happens.
Until recently, the spookiness and excitability were often assumed to be due to the high energy content of the lush grasses. This may indeed still be a contributor, but when looking at all of the symptoms together it becomes clear that another underlying problem exists. The problem is that it is not very clear what this underlying issue is.
Magnesium deficiency has been proposed several times, but most horse nutrition texts give no reference to pasture having the ability to cause a magnesium deficiency, much less that magnesium deficiency is capable of causing all of the symptoms seen.
While this is a topic that one could easily spend years researching without answering many of the questions we now have, the following is my take on pasture induced magnesium deficiency and how it may be affecting your horse.
Can a magnesium deficiency really cause all of these problems?
The NRC 2007 publication reports that magnesium deficiency may cause ‘nervousness, muscle tremors and ataxia (incoordination), with the potential for collapse, hyperpnea (deep breathing) and death’. It goes on to say that ‘while uncommon, tetany in transported horses has been attributed to hypocalcaemia and potentially hypomagnesemia’. The NRC 1989 publication also stated that ‘pastures that are conducive to magnesium deficiency, tetany and death in ruminants do not affect horses similarly’. It then goes on to say that ‘no evidence was found in the literature to support this claim’. I am pointing this out only to demonstrate how little is known about this condition in horses. On reading this information about magnesium it would be easy to assume that a pasture induced magnesium deficiency in horses would be a rare occurrence.
The fact is, many horse people are reporting strange behaviour in horses during the times of year pasture is young, green, lush and rapidly growing so something is going on. With such little information available in horses on magnesium deficiency, we must again look to other animal species for clues.
It is quite well documented in ruminant animals that during phases of grass tetany (magnesium deficiency, most commonly seen in high producing dairy cows during early lactation grazing lush pastures) that affected animals are nervous with an overly alert appearance, they may lose coordination and ‘stagger’ and they may also become aggressive. Humans are also reported to suffer with cramps and muscle weakness as well as become confused, delusional, disoriented, suffer hallucinations and become aggressive during periods of magnesium deficiency. Hypocalcaemia (low plasma calcium) is also frequently observed in both humans and ruminants with magnesium deficiency. So while we don’t have direct, documented evidence in horses (yet), certainly the symptoms we are seeing in horses relate well to symptoms seen in other animal species under conditions of magnesium deficiency.
(The effects of magnesium deficiency in humans are far more extensive than listed above.)
The Science – why are these symptoms present?
OK, so here we go with some of the underlying science to these problems that will help to explain why a magnesium deficiency can cause the symptoms seen in horses.
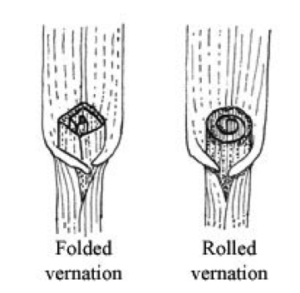
Magnesium is essential for the functioning of a magnesium dependent enzyme called acetylcholine esterase. Acetylcholine esterase is needed for the breakdown of the neurotransmitter acetylcholine. During periods of magnesium deficiency, acetylcholine esterase does not function as it should and acetylcholine accumulates at the motor end plates causing neuromuscular excitability. This accumulation of acetylcholine is likely to contribute to the tense muscles, incoordination, muscle twitches and spookiness seen in magnesium deficient animals.
Magnesium is also needed for the adenyl cyclase enzyme which is involved in the action of parathyroid hormone. This compromised function of the parathyroid hormone (PTH) is thought to be the main cause of hypocalcemia which is commonly observed in magnesium deficient animal species including ruminants, humans and rats as PTH is needed for calcium absorption. PTH is also needed for magnesium absorption, so magnesium deficiency predisposes an animal to a more severe magnesium deficiency by altering the function of the hormone needed for its absorption.
Magnesium is required for the phosphorylation of vitamin B1 (thiamine) into the biologically active thiamine pyrophosphate, so in effect a magnesium deficiency will cause a vitamin B1 deficiency, even when there is ample vitamin B1 in the diet. In humans, a vitamin B1 deficiency can cause confusion, and disorientation with sufferers reportedly becoming delusional and even hallucinating (maybe your horse really does see goblins hiding behind the tree!). Vitamin B1 deficiency can also lead to aggression. In horses, vitamin B1 deficiency is known to cause loss of appetite, incoordination, muscle twitching, tremors or stiffness, overflexing of the hindlegs, unnatural extension of the forelegs and hypothermia (low temperature) of the bodies extremities like the legs, muzzle and ears. Thiamine deficiency may also result in missed heart beats and lactate accumulation in the muscles.
Finally, a magnesium deficiency affects nitric oxide production by motor neurons. In situations of low extracellular nitric oxide but high intracellular nitric oxide in humans, aggression can result.
This by no means is a complete review of how a magnesium deficiency may affect horses and again it is a subject I would need to research for years to fully understand (as there is some serious biochemistry involved). This mini review should however serve to demonstrate that should a magnesium deficiency occur, it is certainly capable of producing the varied symptoms being observed in horses by their owners.
How does it happen?
So, now that we know a magnesium deficiency could be the root cause of the unusual symptoms and behaviours observed in horses grazing lush, green and rapidly growing pastures, let’s look at what it is about these pastures that can cause a magnesium deficiency.
Reduced Magnesium Absorption
Lush, young, rapidly growing pastures are well known to have high potassium and low magnesium levels. While direct evidence for horses is not available to my knowledge, in ruminant animals it is well known that excessive potassium can reduce the absorption of magnesium from the rumen. High dietary potassium is also reported to reduce magnesium absorption in humans. While it is only through extrapolating from data in other animal species, it is likely that excessive potassium in the equine diet also reduces the absorption of magnesium in horses. This reduced absorption, coupled with an already low magnesium concentration in the diet could possibly result in an induced magnesium deficiency, even if there appears to be enough magnesium in the diet to meet requirements.
The acid base balance of the body can also affect parathyroid hormone (PTH) release, with an alkaline body pH, which commonly occurs on high potassium diets, suppressing the release of PTH in some animal species … so maybe this is also playing a role … and maybe even supplementing magnesium help as the horse may not be able to absorb it due to low PTH levels.
Other dietary factors than can reduce magnesium deficiency include excess calcium (high dietary calcium reduces parathyroid hormone (PTH) release. As discussed above, PTH is needed for magnesium absorption), excess phosphorus (phosphorus can block the absorption of magnesium as it can calcium) or a vitamin D deficiency (also needed for magnesium absorption), vitamin B1 deficiency (affects magnesium absorption by altering the pH environment of the stomach) or vitamin B6 deficiency.
Increased Magnesium excretion from the body
High dietary potassium in lush green pastures not only reduces magnesium absorption in animals, but it can also increase the amount of magnesium excreted from the body, giving it a ‘double-whammy’ effect in causing magnesium deficiency.
In addition, under the right environmental conditions lush green pastures can also have large amounts of nitrate accumulated in their leaves, especially when plants are very young and in the one or two leaf stage. In order to remove nitrate from the body, ruminants and horses bond the nitrate to a cation (a positively charged ion which includes calcium, magnesium, sodium and potassium) to form an ionic complex which is then excreted. Professor T.W. Swerczek, a researcher with the Department of Veterinary Science at the University of Kentucky, USA has reported that when a sodium deficiency exists (which is common in grass-based pastures) nitrate is more likely to bond with calcium or magnesium, so under high nitrate conditions, a magnesium deficiency can occur.
Other factors that may increase magnesium excretion from the body include excess oestrogen (possibly putting mare’s or horses grazing estrogenic forages like some clovers at higher risk) and a dietary selenium deficiency (again this is not confirmed in horses but is taken from human data).
So, with the combination of factors that reduce magnesium absorption and increase magnesium excretion from the body, a magnesium deficiency is certainly possible under the right conditions for horses grazing lush, green, rapidly growing pastures.
Do endophyte mycotoxins play a role?
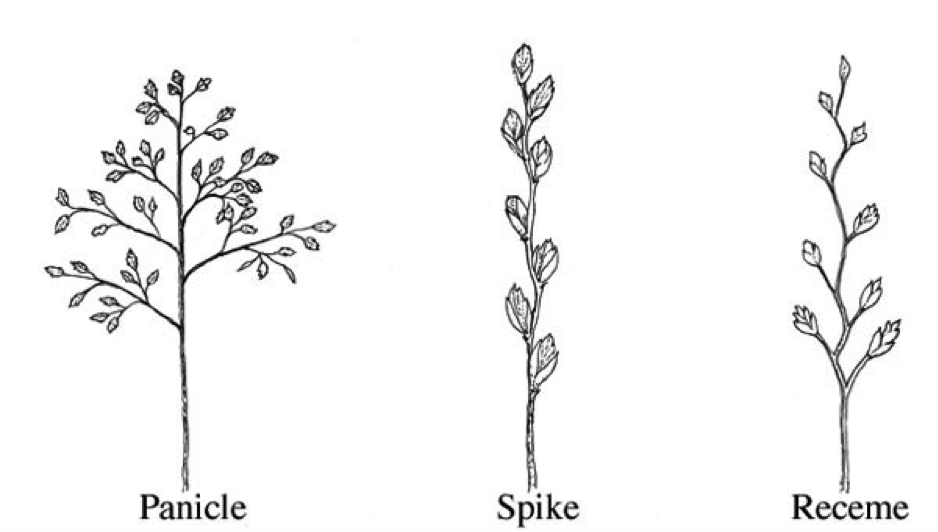
They certainly could, though they need not be present for the symptoms of magnesium deficiency to appear. Ryegrass and fescue pastures that are infected with endophyte fungi may be more likely to contain higher concentrations of the problematic mycotoxins under high pasture potassium conditions (Swerczek 2003). Knowing whether or not they are involved is however going to be tricky as many of the symptoms of endophyte mycotoxicosis are very similar to those that could be caused by magnesium deficiency. Mycotoxicosis is however reported to be most likely when pastures are grazed down to the ground or when they are tall and rank, so it is less likely when the pastures are green, lush and growing rapidly.
Laminitis
Laminitis is often seen in horses during spring and autumn seasons when pastures are green, lush and growing rapidly. It is now known that insulin resistance and high levels of circulating insulin are the most likely cause for most pasture based cases of laminitis and this certainly does help to explain most cases. However, rapidly growing pastures and particularly rapidly growing pastures in warmer climates are unlikely to have large amounts of accumulated sugars and starches and yet laminitis can still be found on these pastures. So, if it isn’t sugar and starch causing the laminitis, what is?
Insulin is used as a signal to cells to take in potassium from the blood. A really interesting study in cows and calves by Lentz et al (1976) found that high levels of potassium (infused as potassium chloride) caused significant elevations in plasma insulin and in the calves, this response was further exaggerated in magnesium deficient animals. So it is quite possible that the high potassium content of lush pastures coupled with an induced magnesium deficiency is causing laminitis by causing prolonged elevations of insulin, which presumably would be worse in insulin resistant animals. This would certainly make a very worthy avenue of research.
It is also possible that the high nitrate levels that can accumulate under the right environmental conditions in young, lush, green pastures leads to laminitis. There is gathering anecdotal evidence to support this theory but as yet no science to actually prove it.
Further, research by Paolisso et al, published in the American Journal of Clinical Nutrition (1992) showed that administering magnesium to elderly patients at a rate of 4.5 g/day improved their glucose handling and insulin sensitivity. This finding begs the question of whether a transient magnesium deficiency that may occur in horses when grazing rapidly growing spring or autumn pastures increases the risk of laminitis for already insulin resistant horses during these periods by exacerbating their insulin resistant status.
What can you do about it?
While there may not be much published equine evidence to prove all of this is happening with your horse, if your horse is showing symptoms that could be related to a pasture induced magnesium deficiency there are some things you can do to help, including:
- Seek veterinary advice if your horse is showing symptoms – magnesium deficiency to the point where an animal is showing symptoms is a serious medical condition and you should always consult your veterinarian for advice. Your horse may be deficient to the point where magnesium and calcium need to be administered parenterally to restore blood levels back to a point that will alleviate the most severe symptoms and also allow magnesium and calcium to be absorbed from the gastrointestinal tract again (as very low magnesium levels turn down parathyroid hormone levels which then reduces magnesium and calcium absorption). It may be a good idea to discuss testing your horse’s level of parathyroid hormone as part of your vets overall assessment of your horse’s condition.
-
Remove animals from problem pasture – if it is possible, you should remove your horse from the problem pasture as soon as any signs are evident. Or if you know your pastures are problematic at certain times of the year, plan in advance and have them off the pastures before the symptoms appear.
If you are unable to remove your horse from the pasture completely you should somehow try to restrict intake of the pasture by using a grazing muzzle during certain periods of the day (if laminitis due to sugars isn’t a concern then muzzling overnight and early in the morning is suggested as this is when nitrate levels are highest) or by strip grazing the pasture in small amounts each day and providing a low potassium forage like a mature grass/meadow hay. - Use a low potassium forage as the base of the diet – mature grass hay will provide you with a lower potassium alternative to the lush pasture. If your horse is already suffering symptoms you should also soak the hay for 30 minutes to remove as much potassium from the diet as you can.
-
Supplement with magnesium, calcium, sodium and vitamin B1 – This is where it gets tricky as while we know you should supplement with these nutrients it is hard to say how much more you should add to the diet. Luckily though, all of these nutrients have a wide safety margin, so we are afforded a nice big safety net.
For a horse suffering with symptoms of magnesium deficiency, I would provide the following: Magnesium, sodium and vitamin B1 – an additional 100% of the recommended daily intake for your horse.
Calcium – in theory, once you have corrected the magnesium deficiency and get the parathyroid hormone functioning as it should again you shouldn’t need to add additional calcium to the diet if the amount in the diet is already adequate. However, if your calcium to magnesium ratio in the diet is less than 2 parts calcium to one part magnesium on addition of the extra magnesium you should add enough calcium to bring this ratio back up to 2: 1. - Correct any deficiency of vitamin B6 and selenium that may exist in the diet – A deficiency of these nutrients leads to reduced magnesium absorption and increased magnesium excretion, so it makes sense to ensure your horse’s requirements are met according to the FeedXL recommended daily intakes for these nutrients.
- Avoid pastures, feeds and conserved forages that may contain oestrogens – Excess oestrogen reportedly increases magnesium excretion from the body so it would make sense to keep the dietary intake of plant derived phytoestrogens to a minimum during high risk periods of pasture induced magnesium deficiency. This includes avoiding clover, alfalfa/lucerne and feeds that contain soybean or soybean meal. These feed ingredients also tend to contain large amounts of potassium so avoiding them provides a double benefit (please note though that under normal circumstances all of these ingredients can play a valuable role in a horse’s diet so don’t go overboard in avoiding them all the time).
- Learn to recognise high risk periods and either remove your horse from the pasture or begin magnesium, sodium and vitamin B1 supplementation early – Pastures are high in potassium and nitrates during rapid, early stages of growth which can be seen during any time of the year depending on the climate where your horse lives. Particularly high risk periods include pasture growth associated with drought breaking rains, frost periods, cloudy days, hot dry winds and cold weather. Any of these (very varied) climatic conditions can induce high potassium levels, high nitrate levels or both in pasture where soil potassium and nitrate is plentiful
- PLEASE don’t ride your horse – if your horse is showing symptoms of magnesium deficiency please don’t try to ride. Your horse in this condition is both physically and mentally unstable and trying to ride would be the safety equivalent of getting into a car with a seriously drunk person and going for a drive – it really isn’t worth the risk and it won’t be enjoyable for you or your horse.
A very real, but not very well recognised syndrome
Having seen some severe cases over the last few years there is no doubting that this condition exists, but as yet it isn’t recognised in nutrition texts. While it may seem like a simple matter of adding extra magnesium to the diet to correct the issue it isn’t that easy as the various factors discussed above may be contributing to low magnesium absorption or high magnesium excretion rates. If your horse is exhibiting these symptoms or other unusual behaviour that you think may be linked to your pasture you should have your pasture analysed to determine mineral levels you are working with and work closely with your vet and FeedXL to get your horse’s diet rebalanced and your horse’s magnesium levels restored.
Join FeedXL today and take control of your horse’s nutrition
Get EVEN MORE practical and personalised feeding guidance when you sign up to FEEDXL.
Do you have a question or comment? Do you need help with feeding?
We would love to welcome you to our FeedXL Horse Nutrition Facebook Group. Ask questions and have them answered by PhD and Masters qualified equine nutritionists and spend time with like-minded horse owners. It’s free!
Click here to join the FeedXL Horse Nutrition Facebook Group