Avoiding Gastric Ulcers in Horses
Equine Gastric Ulcers: Feeding management strategies to reduce the risk for your horse
Equine gastric ulcer syndrome (EGUS) is a major equine health problem worldwide. Multiple studies have reported an incidence of ulcers in performance horses in excess of 90% of horses training.
Ulcers negatively – and sometimes severely – affect a horse’s ability to perform. They cause pain and discomfort. They may reduce a horse’s appetite which in turn limits its capacity to maintain bodyweight. Gastric ulcers can also possibly lead to the development of vices including windsucking and crib biting.
While gastric ulcers in horses have long been recognised as a major health concern, there is an evident lack of understanding in the horse community about what causes them and how they can be prevented.
Continue reading to find out a little bit more about what gastric ulcers are, how your horse’s stomach functions, and a few little things you can do that will dramatically reduce the risk of your horse’s stomach developing this painful condition.
What are Gastric Ulcers?
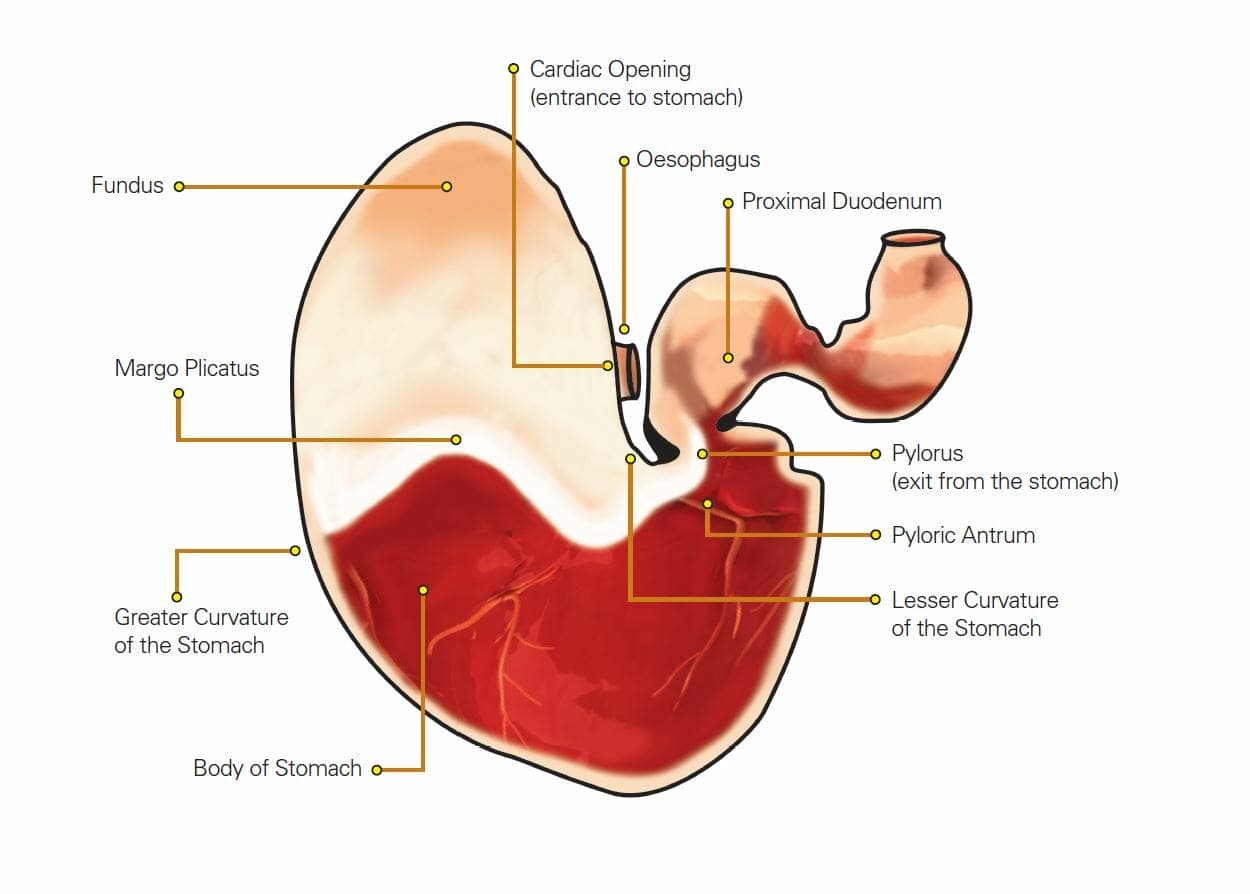
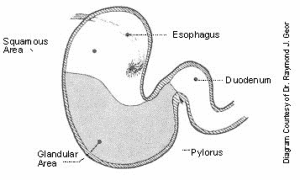
Gastric ulcers are lesions that are found in the stomach of horses. The horse’s stomach is made up of 2 major regions, the upper ‘squamous’ area and the lower ‘glandular’ area. Gastric ulcers are categorised by their location in the stomach being either squamous gastric ulcers or glandular gastric ulcers – these are two distinct diseases with different risk factors.
Why do gastric ulcers occur in the squamous or upper section of the stomach?
The horse evolved as a grazing animal and, when left to their own devices, will eat for 17 hours or more per day. This means they are constantly chewing and salivating, and their stomach is always full. Because of this pattern of eating, their stomach never developed an on-off-switch for gastric acid production. The equine stomach secretes gastric acid 24-hours a day, regardless of whether they are actually eating or not.
When you think about this from the perspective of our modern-day horses, it is not an ideal situation. Many horses are now stabled with limited access to free choice forage, or they work, compete, and travel, leaving them in situations where they go for extended periods of time without feed.
When a horse eats it produces saliva and one of saliva’s roles is to buffer the gastric acid in the stomach. So, when they aren’t eating, they aren’t salivating. BUT they are still secreting gastric acid. This results in a pool of unbuffered (and therefore very acidic) gastric fluid accumulating in the lower section of the horse’s now empty stomach.
The lower part of the horse’s stomach was smart enough to protect itself from gastric acids, and, provided it is well-nourished, is able to produce enough sticky mucous to protect itself from its own acid secretions. BUT, the upper part of the stomach doesn’t have this same protection. In a grazing horse, the stomach is always full, so the top of the stomach was never exposed to gastric acid simply because the forage a horse ate stopped the acid from ever splashing up there. However, in modern-day, meal-fed horses, the stomach is often empty and the upper section of the stomach is left totally exposed to the highly acidic fluids that are allowed to accumulate in empty stomachs.
When a horse with an empty stomach trots, canters, gallops, or even simply tenses up its abdominal muscles the gastric fluids are splashed or squeezed up onto the unprotected upper section of the stomach. Simply put, the acid starts to burn holes in the stomach wall lining. If you allow this to occur repeatedly, the horse will eventually develop ulcers. This can happen in just a matter of days.
What major factors influence the risk of squamous gastric ulcers?
The following situations have been identified as factors that can influence the risk of squamous gastric ulcers:
- Low forage intake – Not having free access to forage and not being provided with additional forage increases the risk of squamous ulcers (Gehlen et al., 2019).
- Feeding Frequency – Feed deprivation such as might occur during transport and long periods between meals lowers the pH in the equine stomach and allows the stomach to empty, both of which will increase the risk of gastric ulceration (Murray, 1994).
- High starch diet – Horses receiving large proportions of grain (or starch) in their diets are at increased risk of squamous ulcers (Gehlen et al., 2019). One study shows that a reduction in dietary starch resulted in a decrease in squamous ulcers (Böhm et al., 2018).
- Exercise – As a horse exercises, the pressure inside the stomach increases, which forces the highly acidic gastric contents from the glandular area up into the unprotected squamous area (Lorenzo-Figueras et al. 2002). Horses in training are known to have a higher incidence and also more severe gastric ulceration than horses not in work. Similarly, the intensity of long-duration exercise also increases the risk and severity of squamous ulcers in both Thoroughbred racehorses (Murray et al., 1996) and endurance horses (Tamzali et al., 2011).
How can feeding management reduce the risk of squamous ulcers?
Some feeding management practices that may help reduce the incidence of squamous ulcers are:
- Don’t exercise horses on an empty stomach – Providing 1-2kg of lucerne hay prior to exercise helps to prevent acidic contents from the lower region of the stomach from splashing up onto the upper region where it can cause squamous ulcers. The saliva created while chewing the hay also helps to buffer the acidity in the stomach. Using lucerne hay has the extra positive benefit with the buffering effect from the high content of protein and calcium in lucerne itself. If you don’t have or feed alfalfa (lucerne) hay, then your horse’s regular hay will also work well.
- Provide constant access to pasture or hay – Allowing the horse to feed continuously during the day and night will help to reduce the likelihood of squamous gastric ulcers developing. However, free access to forage does not always guarantee your horse is eating enough forage. For example, overgrazed pasture (<2.5cm or 1 inch in height) does not provide adequate amounts of fibre to protect the stomach. Likewise, providing free access to a round bale does not guarantee your horse is consuming adequate amounts. This may be due palatability of the hay or an already depressed appetite from gastric ulcers. Horses need to be consuming at least 1.5 to 2% bodyweight in forage per day. Providing supplementary hay to horses on pasture and feeding a set amount of hay per day is the easiest way to ensure adequate intake.The importance of constant access to adequate amounts of forage ensures good amounts of saliva being produced by chewing, which has a buffering effect on stomach acid, and fibre’s ability to create a ‘ball’ in the stomach to limit acid splashing. If horses need to go periods without access to forage or having a feed, this should be limited to no more than 5 hours.
If you are travelling long distances with your horse, and it is safe to do so, providing hay in a hay net during travel will provide the horse with an opportunity to continue eating during transport. If this is not possible, take regular breaks and provide small forage meals during the trip.
- Reduce starch in feeds – Reducing the amount of starch in the diet by reducing or removing grain-based concentrate from feeds is recommended. Due to the different starch content of various grains and feeds, maximum intakes are based off starch intake. No more than 1 gram of starch per kilogram of bodyweight per meal should be fed and maximum of 2 grams of starch per kilogram of bodyweight per day. For example, barley contains on average 60% starch. For a 500kg horse, the maximum amount of barley which should be fed is 800g per meal or 1.6kg per day split over two meals, which is the equivalent of 480g of starch per meal.For horses requiring a high energy diet, grain-based feeds can be substituted with a combination of high energy fibre such as alfalfa pellets, chaff or alike, beet pulp, soybean hulls, and high fat ingredients such as oilseeds and oils.
What about Glandular ulcers?
The following situations have been identified as potential risk factors for glandular ulcers:
- Exercising more than 4 days per week – Exercising 5 or more days per week was a key risk factor for glandular ulcers in Thoroughbred racehorses (Sykes et al., 2019). Another study showed that increased days in work (up to 6 days per week) and actively competing are risk factors in Warmblood showjumpers (Pedersen et al., 2018). The prevalence of glandular ulcers doubles in in endurance horses during competition season (Tamzali et al., 2011). It’s not clear why exercising for 5 or more days per weeks increases the risk of glandular ulcers, although it is hypothesised that during exercise there is a decrease in blood flow to the stomach (Rendle et al., 2018).
- Stress – an increased prevalence has been observed in domesticated horses compared with feral horses (Ward et al., 2015). This suggests that intensive management plays a role in the increased risk of glandular ulcers in horses. Stabling or confinement, lack of contact with other horses (individually paddocked), and having multiple handlers or riders can all increase risk.
How can feeding management reducing the risk of glandular ulcers?
Diet does not appear to a key risk factor but does form part of the management of horses at risk of glandular ulcers. One study looking at the effect of diet composition on glandular ulcers does support this (Julliand et al., 2023). Some of the key findings of this study were:
- Horses allocated to the non-ulcerated group had a higher daily intake of simple sugars in their pre-Day 0 diet (same diet for 4 weeks prior to Day 0) than horses in the ulcerated group.
- Horses which remained on the full rate of grain concentrate did not show improvement in glandular scores over the 42-day study period. In fact, the number of horses with glandular ulcers greater than 2, increased over the study period.
- Five out of six horses that had half their grain concentrate substituted with alfalfa pellets showed improvement in their glandular scores from greater than 2 to scores of 0-1.
Some feeding management practices that may help reduce the incidence and severity of glandular ulcers are:
- Reduce starch in feeds – This is beneficial for reducing the fermentation products in the gastric contents which, when combined with a very acidic environment, cause damage to the glandular mucosa. For horses requiring a high energy diet, this can be achieved by substituting grain-based feeds with a combination of high energy fibre feeds like beet pulp, soybean hulls, etc and high fat ingredients such as oilseeds and oils.
- Include alfalfa (lucerne) in feeds – Inclusion of alfalfa (lucerne) pellets, chaff or alike with grain concentrate can provide a buffering effect within the stomach to maintain a higher pH, reducing harmful effects of short chain fatty acids on gastric mucosa.
In the above-mentioned study, horses receiving approximately 5-6kg of grain concentrate per day transitioned to a diet of approximately 3kg grain concentrate and 2.8kg of alfalfa pellets per day. As a guide, inclusion of 2-2.5kg of alfalfa (lucerne) pellets or alike to feeds may be beneficial.
If your horse already has gastric ulcers, you must treat them
While one study has shown that feeding lucerne hay can reduce the severity of ulcers already present in horses and long periods of pasture turnout will sometimes allow a horse to resolve gastric ulcer issues, if your horse already has gastric ulcers, treating them with veterinary prescribed medication is important for a quick resolution. Talk to your veterinarian about the best treatment regime for your horse.
Finally …
Gastric ulcers are a serious and common health problem in horses that will affect their overall wellbeing and performance. While we still don’t have a full understanding of how and why they occur with such a high incidence, using the feeding and management strategies outlined above will help to reduce your horse’s risk of developing gastric ulceration.
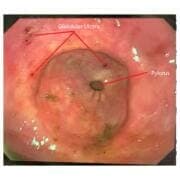
Image provided by RandLab (https://www.randlab.com.au)
Do you have a question or comment? Do you need help with feeding?
We would love to welcome you to our FeedXL Horse Nutrition Facebook Group. Ask questions and have them answered by PhD and Masters qualified equine nutritionists and spend time with like-minded horse owners. It’s free!
Click here to join the FeedXL Horse Nutrition Facebook Group